Onur Asan: Division of General Internal Medicine, Center for Patient Care and Outcomes Research, Medical College of Wisconsin, Milwaukee, WI, USA
Enid Montague: Division of General Internal Medicine and Geriatrics, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Cite this article: Asan O, Montague E. Using videobased observation research methods in primary care health encounters to evaluate complex interactions. Inform Prim Care. 2014;21(4):161–170.
Copyright © 2014 The Author(s). Published by BCS, The Chartered Institute for IT under Creative Commons license http://creativecommons.org/licenses/by/4.0/.
Abstract
Objective The purpose of this article is to describe the use of video-based observation research methods in primary care environment and highlight important methodological considerations and provide practical guidance for primary care and human factors researchers conducting video studies to understand patient–clinician interaction in primary care settings.
Methods We reviewed studies in the literature which used video methods in health care research, and we also used our own experience based on the video studies we conducted in primary care settings.
Results This article highlighted the benefits of using video techniques, such as multi-channel recording and video coding, and compared “unmanned” video recording with the traditional observation method in primary care research. We proposed a list that can be followed step by step to conduct an effective video study in a primary care setting for a given problem. This article also described obstacles, researchers should anticipate when using video recording methods in future studies.
Conclusion With the new technological improvements, video-based observation research is becoming a promising method in primary care and HFE research. Video recording has been under-utilised as a data collection tool because of confidentiality and privacy issues. However, it has many benefits as opposed to traditional observations, and recent studies using video recording methods have introduced new research areas and approaches.
Keywords: observations, primary care research, video recording
Introduction
The health care system is complex and involves a range of people from various backgrounds and perspectives who communicate, interact and collaborate. Several US Institute of Medicine (IOM) reports have addressed major problems in healthcare delivery, such as medical errors, poorly designed medical technologies and poorly designed work environments.1 To this end, an IOM report proposed a partnership between health care and industrial and system engineering, including human factors engineering (HFE), to create solutions for these problems.2 HFE is the study of interactions of humans with the systems, products and environment and takes a system approach to study interactions.3 Primary care is one of the main components of the health care system and involves the widest scope of health care, including a variety of demographics, such as patients of different ages and socioeconomic backgrounds, as well as patients with different kinds of chronic and acute health problems.4 There are several HFE issues specific to the primary care environment, which human factors researchers can address with various methods. Some of them are related to information processing, standardisation, simplification, work pressure and work load, organisational design, information access, technology acceptance, usability and the effect of EHR use on doctor–patient interaction.5 a,b Depending on the context, HFE researchers are tasked with determining which components of the system are likely to influence patient outcome measures (for example, satisfaction, trust and adherence to treatment). Therefore, the HFE discipline can play a major role in improving overall primary care health systems leading to better health outcomes.4
Observational research is a commonly used method in primary care studies. However, direct observation is not always the best choice for analysing primary care encounters,6 as it is difficult for researchers to capture all details in a live setting, particularly when components occur simultaneously.7 Video recording may eliminate some of the challenges that occur in direct observation research in a primary care setting,8,9 since video recording accurately records clinical events, allows researchers to verify their observations and allows for the collection of systematic feedback by means of strategic participant review.10 Video data can also give researchers insight into the consistency between self-assessment and observable behaviour. Finally, the video recording of subjects’ ongoing activities in their natural setting11 can also be a particularly useful way to employ ethnographic studies in a complex primary care environment.
However, using video effectively requires the determination of appropriate research questions and identification of types of data required beforehand to inform study design. Video recording research also requires technical knowledge to ensure the appropriate selection of cameras, video quality adjustment and positioning of cameras.12,13 Currently, enhanced video technology allows for richer data and facilitates the data collection process with alternatives such as multi-channel streams and remote-controlled cameras.14,15 It is essential to note that the research purpose may affect the type of technology used in the study design.
This paper outlines the steps for using video methods in a primary care setting. This paper also addresses potential benefits of using video observation and video analysis methods, which can be used by human factors and health care researchers in primary care settings.
Background on the use of video recording in primary care research
Primary care researchers began using video recordings to study consultations in the late 1970s.16 In one early study, a communication analyst videotaped primary care consultations with a single video camera and subsequently analysed the communication patterns between doctors and patients to improve doctors’ communication skills.17 The results showed that doctors’ communication styles affected patient satisfaction. Recent studies have used video data to analyse non-verbal communication cues to inform more effective doctor–patient interactions.18–20 Video data were also utilised to train doctors to improve their interactions with patients.16 In addition, studies have used video recordings to explore doctor–patient–computer interactions.21–29 These studies were instrumental in identifying the best spatial organisation of an exam room, better design of exam-room computers, impact of computer use on communication and effective use of the computer by the doctor during the clinical visit. Several studies also utilised video elicitation interviews (which are basically interviews done after the recording, asking the doctors or patients to reflect on what they see on the video) to analyse doctor–patient interaction in the visits for teaching purposes.30,31 Video elicitation allowed researchers to integrate the data from the video recording and participants’ related thoughts, beliefs and emotions obtained from the elicitation interviews.32 Although traditional observation can provide a range of interesting and insightful information about primary care encounters, the encounter occurs through complex and multiple interactions that can be explored by video data better. Finally, video data have also been used in health care settings in addition to primary care consultation for various purposes.33
Considerations for collecting Video Data in Primary Care
Video-recording methods require careful planning in order to gather data that effectively answer potential research questions. Table 1, which is derived from our experience of several studies,26–28 summarizes the steps to conduct a video observation study in a primary care setting for a given problem.
Some of the elements listed in different categories in Table 1 have inter-dependent nature, for instance, number of participants, time frame of the study, time needed for ethical approval and the instruments may all have mutual effect. Furthermore, video data might have ‘identifiable private information’ and involve human subject data, therefore require some additional requirements for IRB review.34 In video data collection, compared with traditional observation, studies conducted in US showed that physicians might have concerns about potential liability.35 Therefore, there should be a consensus between administrators and investigators about the purpose of the research and the methods used. Studies in US reported that it can also be effective to have some strategies to overcome doctors’ concerns with confidentiality and liability, such as obtaining certificates of confidentiality36 or becoming familiar with the liability coverage at the clinic where data will be collected.37 As added protection, a previous study reported that patients were generally less worried than doctors about being videotaped.32 However, it is still essential to get certificates of confidentiality to protect the participants’ identifiable information from forced disclosure. IRB approval requires confidentiality, but in the case of some sort of legal case (such as a malpractice case), the court might be able to force researchers to reveal this information. Certificates of confidentiality – which allow the investigator and others who have access to research records to refuse to disclose identifying information on research participants in any civil, criminal, administrative, legislative or other proceeding, whether at the federal, state or local level – might prevent this potential conflict between IRB and legal jurisdictions with respect to discoverability.38
Table 1 Steps followed to conduct this video study

With technological advancements, some researchers have started to use more complex video methods for data collection to capture all interactions in detail – such as body language and gazing direction.9,14,39 A multi-channel video might be a superior method to single-channel video depending on research question as it collects a greater amount of information, allowing the research to see both the care-provider and the patient simultaneously from different angles.14 For instance, some researches created a multi-channel video technique and software to capture all the computer use (including screen-capture, key stroke and mouse movement), and doctor–patient interaction in detail, which enabled them to view simultaneously all data relating to any time or activity.25 Another study used multi-channel video recording focussing on the patient’s face, the physician’s face and the overall interaction to capture eye gaze patterns.27,28
Furthermore, as video recording technology becomes more complex, researchers are faced with a wide variety of options, so it is important to choose the methods and equipment best suited to a given study. Researchers should standardise the camera operation protocols and have back up cameras in case of malfunctioning. In addition, multi-channel video and audio recording can collect so much data that the process of analysis becomes more complicated and time consuming. Therefore, it is essential to determine the specific research problems to minimise data collection and analysis time.
The Benefits & Drawbacks of Video Methods
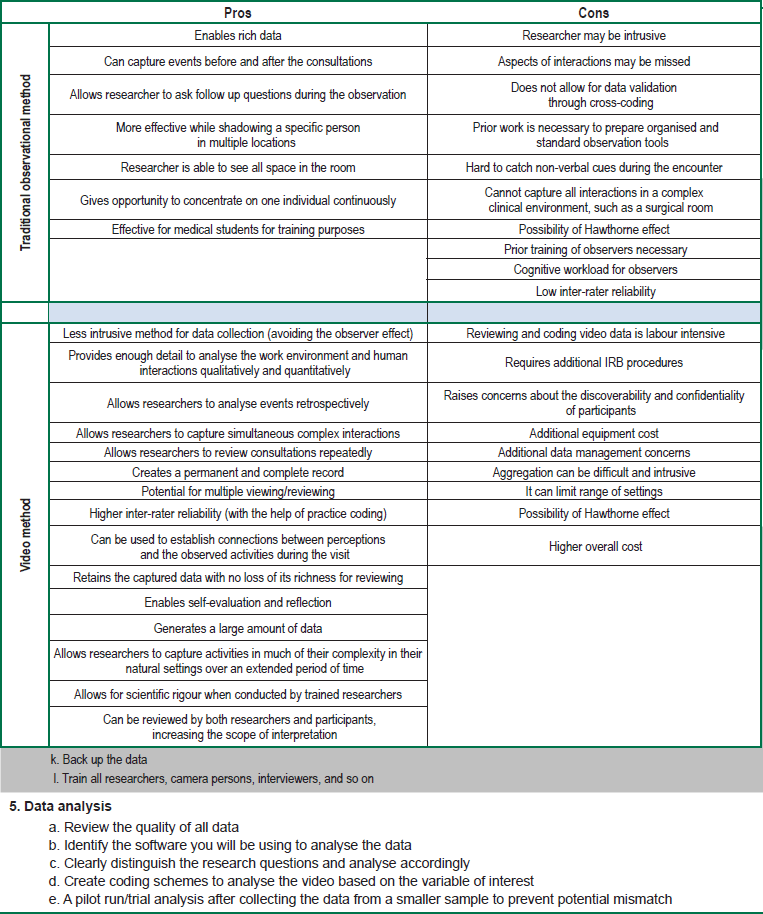
Table 2 shows the pros and cons of traditional human observation method and video recording by ‘unmanned’ cameras. This table was established based on our own experience and previous studies.6,7,36,37,39,40–42
Video methods can be effective for research that can be conducted in a single room (for example, the patient exam room in a primary care clinic), since the cameras can be set up in a fixed position, specifically focussing on the interaction in the exam room. In addition, cameras can also be used in various ways based on research questions because cameras can be carried, placed in multiple rooms or cameras’ angle can be changed in real-time by remote control. When the required conditions are met, the video method can provide a rich collection of data. For instance, in one study, we used multiple small cameras with sufficient battery time and SD cards and hooked them on to the walls or side of the desks in the room. Remote control was utilised to start and stop the camera, and a remote control was left with the doctor so the doctor could stop the recording if the patients did not feel comfortable or the conversation topic becomes highly confidential, such as drug use or suicide.
Table 2 The benefits and drawbacks of video method and traditional observational method
Furthermore, video method also limits the Hawthorne effect – which is the possibility of altering the behaviour of participants – since video cameras have been shown to influence participant behaviour far less than a human observer.43 However, some people may be less willing to be videotaped as opposed to live observation and feel there is more risk involved in video data due to several reasons: a) video recordings may be viewed by multiple people over time, b) outsiders may gain access to video data that are improperly stored, and c) a person’s identity may be more readily determined from a video recording than from written data. On the other hand, video data might improve ecological validity, since the video data give more complete (and visual) information about the real environment rather than traditional observers’ observation notes.
Video Data Management & Analysis
Observation data, including both video and non-video data, are confidential. However, video data introduce more risk to overall confidentiality because video data keep all interaction in a high fidelity format for several years and might be accessed by multiple people for research or non-research purposes unless sufficient precautions are taken. Video data should be stored on a secure storage without links to other identifiable information, such as address, name and social security number.32
Coding is a standard procedure to analyse the video data. Coding is an established procedure that facilitates analysing the video by identifying the tasks and interactions in the video.19 A coding scheme classifies variables of interest in the video according to the purpose of the analysis, and it speeds up the coding process. Development of coding scheme should be informed by the literature.45 Each variable in the coding scheme should be well defined, and the start and stop time of all variables should be standardised. This may help to improve the reliability of data coding and decrease biases of different coders. For example, in one study, coders were interested in the gaze direction of the doctor and patient 46 and created a coding scheme including the subject (patient or doctor) and the object of the gaze (patient, care provider, computer, chart, and so on.). This scheme allowed for a thorough and specific analysis of gaze based on subject, object and duration, such as total duration of doctor’s gaze at computer and patient during a visit.
Video data can be coded both quantitatively and qualitatively depending on the purpose of the research. Quantitative data might include the duration of specific behaviours in the visit. Software packages can help quantify all continuous behaviour (such as gazing or typing) to obtain relevant data with respective time frames.27 It is also possible to visualise the sequence of the behaviours using software. Qualitative analysis might be a thematic description of a practitioner’s behaviour during the entire visit, such as patient-focussed or computer-focussed. Qualitative data might also be gathered based on verbal communication, such as analysing turn takings and sequence of utterances.18 Some studies also used tools such as check lists (physicians’ behaviour checklist) to capture human performance data from the video recording,47 such as counting the occurrence of specific doctors’ behaviours during the doctor–patient encounter in the video data.48
Video Analysis Tool
Potential Uses of Video Data in Primary Care Research
Evaluating complex constructs and interactions in real, complex and dynamic clinical environments plays an important role in improving health care system; and thus, it is a priority for HFE researchers. Effective functioning of the health care system depends on the interactions among people (patients, physicians and other medical staff) and the interaction between people and technology.4 Therefore, their interactions should be explored in detail to improve overall health care systems. Video data can contribute to studies exploring doctor–patient interaction for different research purposes, such as analysing the decision-making process between doctor and patient,30 determining the effects of non-verbal behaviours between patient and doctor that influence their decisions,31 exploring factors which yield misunderstanding and disagreement during the interactions51 and investigating patients’ responsiveness to specific doctor behaviours.52 One study also reported a list of seven different goals to use video-recorded consultations.39 Furthermore, video data can also contribute to the analysis of people–technology interaction in primary care settings.53 For instance, it is critical to capture accurately both the pathways users take and the errors users commit while conducting a usability test of a mobile device. The traditional observation method might fail to obtain all data related to pathways and errors during real patient encounters, so video recording could record all necessary data from the screen to be analysed. In addition, with the integration of an eye gaze tracker, video data can provide rich information about eye gaze pathways to analyse the usability of medical software programs.
Video data have also been used to create and test a number of different interactions models in the primary care environment.
Video data can also contribute to doctors’ training since it provides an opportunity for doctors to review their own activities.40 Multiple studies have recorded consultations in the primary care environment to assess clinical competence and design educational interventions.14 Video data were also used with simulations for medical education.67 Clinicians’ interaction style with patient and computer during the visit can influence patient outcomes such as satisfaction, trust and adherence,68 so video data analysis can also contribute to teaching medical students better ways of interacting with patients and EHRs during the encounter.
Video Data and Sociotechnical Design
The components of a sociotechnical system include the individual (such as health care workers), tasks, tools and technologies, the physical environment and organisational conditions.69 It is essential to understand users of the system and interactions among these users in real settings to address sociotechnical design concerns.70 It is also necessary to better understand the impact of boundaries on sociotechnical systems and their implications for physical, cognitive and psychosocial ergonomics. Furthermore, effective design, implementation and use of newly introduced technologies into the overall system is strongly related to the fundamentals of human factors ergonomics.71 A number of studies have focussed on the concept of sociotechnical factors that complicate health information systems deployment,72 including the interaction between the technical features of a health information system and the social features of a health care work environment.73 After a new system implementation, sociotechnical interactions have a direct effect on the success of the process. In the future, many new medical technologies will be introduced into the system. Video recording might also be a strong tool to explore technology interventions, which can make sociotechnical systems more effective and efficient. For instance, video data can be used to analyse the current medical technology, such as electronic health records (EHR) and to inform how new EHR can be integrated into the sociotechnical system more effectively.
Conclusion
Video-based observation research is a promising method in primary care and HFE research. Video recording has been under-utilised as a data collection tool because of confidentiality and privacy issues. However, it has many benefits, and recent studies using video recording methods have introduced new research areas and approaches. There are several possible applications of video recording in HFE and sociotechnical research as well as in traditional clinician training, such as performance evaluation and analysing clinician–patient interactions. This paper is intended to prepare researchers for using video-based observation studies in primary care settings by evaluating the necessary steps involved, including the legal and confidentiality processes, technical aspects, data collection and data analysis and by describing its contribution to human factors research.
A systematic analysis of video recordings gives researchers opportunities to find solutions for human factors-related problems, as well as a sociotechnical systems analysis of interventions in primary care. Video recording method will be increasingly used in future research not only in the health care domain but also in other domains, such as usability and social interaction. Video recording observation studies in primary care environment will continue helping to answer a variety of emerging research questions in primary care.
Acknowledgements
The project described was supported by the Clinical and Translational Science Award (CTSA) programme, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427.
References
- Kohn LT, Corrigan JM and Donaldson MS. To Err is Human: Building a Safer Health System. Atlanta, GA: National Academies Press, 2000.
- Reid PP. Building a Better Delivery System: A New Engineering/Health Care Partnership. Atlanta, GA: National Academy Press, 2005.
- Dul J, Bruder R, Buckle P, Carayon P, Falzon P, Marras WS et al. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics 2012;55(4):377–395. http://dx.doi.org/10.1080/00140139.2012.661087. PMid:22332611.
- Carayon P. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety, Boca Raton, FL: CRC, 2007.
5a. Beasley JW, Hankey TH, Erickson R, Stange KC, Mundt M, Elliott M et al. How many problems do family physicians manage at each encounter? A WReN study. The Annals of Family Medicine 2004;2(5):405–10. http://dx.doi.org/10.1370/afm.94. PMCid:PMC1466713.
5b. Carayon P. Emerging role of human factors and ergonomics in healthcare delivery–A new field of application and influence for the IEA. Work. A Journal of Prevention, Assessment and Rehabilitation 2012;41:5037–40.
- Carthey J. The role of structured observational research in health care. Quality and Safety in Health Care 2003;12(suppl 2):ii13–6. http://dx.doi.org/10.1136/qhc.12.suppl_2.ii13. PMid:14645890; PMCid:PMC1765776.
- Wears RL. Beyond error. Academic Emergency Medicine 2000;7(11):1175–6. http://dx.doi.org/10.1111/j.1553-2712.2000.tb00457.x. PMid:11073460.
- Jeffcott SA and Mackenzie CF. Measuring team performance in healthcare: Review of research and implications for patient safety. Journal of Critical Care 2008;23(2):188–96. http://dx.doi.org/10.1016/j.jcrc.2007.12.005. PMid:18538211.
- Kumarapeli P and de Lusignan S. Using the computer in the clinical consultation; setting the stage, reviewing, recording, and taking actions: multi-channel video study. Journal of the American Medical Informatics Association 2013;20(e1):67–e75. http://dx.doi.org/10.1136/amiajnl-2012-001081. PMid:23242763; PMCid:PMC3715353.
- Seagull FJ and Guerlain S (Eds). Observation Measure of Team Process and Performance in Health Care, Human Factors and Ergonomics Society, 2003.
- Schaeff JH. Videotape: New techniques of observation and analysis in anthropology. Principles of Visual Anthropology 2009:255.
- Theadom A, De Lusignan S, Wilson E and Chan T. Using three-channel video to evaluate the impact of the use of the computer on the patient-centredness of the general practice consultation. Informatics in Primary Care 2003;11(3):149–56. PMid:14680538.
- Sheeler I, Koczan P, Wallage W and de Lusignan S. Low-cost three-channel video for assessment of the clinical consultation. Informatics in Primary Care 2007;15(1):25–31. PMid:17612472.
- Leong A, Koczan P, De Lusignan S and Sheeler I. A framework for comparing video methods used to assess the clinical consultation: a qualitative study. Informatics for Health and Social Care 2006;31(4):255–65. http://dx.doi.org/10.1080/14639230600991668. PMid:17135058.
- Refsum C, Kumarapeli P, Gunaratne A, Dodds R, Hasan A and De Lusignan S. Measuring the impact of different brands of computer systems on the clinical consultation: a pilot study. Informatics in Primary Care 2008;16(2):119–27. PMid:18713528.
- Pilnick A, Hindmarsh J and Gill V. Beyond ‘doctor and patient’: developments in the study of healthcare interactions. Sociology of Health & Illness 2009;31(6):787–802. http://dx.doi.org/10.1111/j.1467-9566.2009.01194.x. PMid:19843267.
- Frankel R. The laying on of hands: aspects of the organization of gaze, touch, and talk in a medical encounter. The social organization of doctor-patient communication. 1983:19–54.
- Bensing JM, Verheul W and van Dulmen AM. Patient anxiety in the medical encounter: a study of verbal and nonverbal communication in general practice. Health Education 2008;108(5):373–83. http://dx.doi.org/10.1108/09654280810899993.
- Zandbelt L, Smets E, Oort F, Godfried M and de Haes H. Patient participation in the medical specialist encounter: does physicians’ patient-centred communication matter? Patient Education and Counseling 2007;65(3):396–406. http://dx.doi.org/10.1016/j.pec.2006.09.011. PMid:17085006.
- Bensing J, Tromp F, Van Dulmen S, van den Brink-Muinen A, Verheul W and Schellevis F. Shifts in doctor-patient communication between 1986 and 2002: a study of videotaped general practice consultations with hypertension patients. BMC Family Practice 2006;7(1):62. http://dx.doi.org/10.1186/1471-2296-7-62. PMid:17064407; PMCid:PMC1630692.
- Pearce C, Kumarpeli P and de Lusignan S. Getting seamless care right from the beginning-integrating computers into the human interaction. Studies in Health Technology and Informatics 2010;155:196. PMid:20543329.
- Frankel R, Altschuler A, George S, Kinsman J, Jimison H, Robertson NR et al. Effects of exam-room computing on clinician-patient communication: a longitudinal qualitative study. Journal of General Internal Medicine 2005;20(8):677–82. http://dx.doi.org/10.1111/j.1525-1497.2005.0163.x. PMid:16050873; PMCid:PMC1490186.
- Pearce C, Dwan K, Arnold M and Phillips C. Analysing the doctor patient computer relationship: the use of video data. Informatics in Primary Care 2006;14(4):221–6. PMid:17504573.
- Pflug B, Kumarapeli P, van Vlymen J, Chan T, Ammenwerth E and de Lusignan S (Eds). Measuring the impact of the computer on the consultation: An application to synchronise multi-channel video, automated monitoring, and rating scales, 2008.
- De Lusignan S, Kumarapeli P, Chan T, Pflug B, Van Vlymen J, Jones B et al. The ALFA (Activity Log Files Aggregation) toolkit: a method for precise observation of the consultation. Journal of Medical Internet Research 2008;10(4). http://dx.doi.org/10.2196/jmir.1080. PMid:18812313; PMCid:PMC2629369.
- Asan O and Montague E. Technology-mediated information sharing between patients and clinicians in primary care encounters. Behaviour & Information Technology 2013(Epub ahead of print):1–12.
- Asan O and Montague E. Physician interactions with electronic health records in primary care. Health Systems 2012;1(2): 96–103. http://dx.doi.org/10.1057/hs.2012.11. PMid:24009982; PMCid:PMC3760434.
- Montague E and Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor–patient communication and attention. International Journal of Medical Informatics 2014;83(3):225–34. http://dx.doi.org/10.1016/j.ijmedinf.2013.11.003. PMid:24380671.
- Kazmi Z. Effects of exam room EHR use on doctor-patient communication: a systematic literature review. Informatics in Primary Care 2014;21(1):30–9. http://dx.doi.org/10.14236/jhi.v21i1.37. PMid:24629654.
- Saba GW, Wong ST, Schillinger D, Fernandez A, Somkin CP, Wilson CC et al. Shared decision making and the experience of partnership in primary care. The Annals of Family Medicine 2006;4(1):54–62. http://dx.doi.org/10.1370/afm.393. PMid:16449397; PMCid:PMC1466999.
- Henry SG, Forman JH, and Fetters MD. ‘How do you know what Aunt Martha looks like?’A video elicitation study exploring tacit clues in doctor–patient interactions. Journal of Evaluation in Clinical Practice 2011;17(5):933–9. http://dx.doi.org/10.1111/j.1365-2753.2010.01628.x. PMid:21210905.
- Henry SG and Fetters MD. Video elicitation interviews: a qualitative research method for investigating physician-patient interactions. The Annals of Family Medicine 2012;10(2):118–25. http://dx.doi.org/10.1370/afm.1339. PMid:22412003; PMCid:PMC3315127.
- Iedema R, Forsyth R, Georgiou A, Braithwaite J and Westbrook J. Video research in health. Qualitative Research Journal 2006; 6(2):15–30. http://dx.doi.org/10.3316/QRJ0602015.
- Menikoff J. Where’s the Law-Uncovering the Truth about IRBs and Censorship. Northwestern University Law Review 2007;101:791.
- Guerlain S, Turrentine B, Adams R and Calland JF. Using video data for the analysis and training of medical personnel. Cognition, Technology and Work 2004;6(3):131–8. http://dx.doi.org/10.1007/s10111-004-0154-2.
- Broyles L, Tate J and Happ M. Videorecording in clinical research: mapping the ethical terrain. Nursing Research 2008;57(1):59.
- Weinger M, Gonzales D, Slagle J and Syeed M. Video capture of clinical care to enhance patient safety. Quality and Safety in Health Care 2004;13(2):136.
- Wolf LE, Zandecki J and Lo B. The certificate of confidentiality application: a view from the NIH Institutes. IRB: Ethics and Human Research 2004;26(1):14–8. http://dx.doi.org/10.2307/3563582. PMid:15281213.
- Coleman T. Using video-recorded consultations for research in primary care: advantages and limitations. Family Practice 2000;17(5):422. http://dx.doi.org/10.1093/fampra/17.5.422. PMid:11021903.
- Mackenzie C and Xiao Y. Video techniques and data compared with observation in emergency trauma care. Quality and Safety in Health Care 2003;12(suppl 2):ii51. http://dx.doi.org/10.1136/qhc.12.suppl_2.ii51. PMid:14645896; PMCid:PMC1765775.
- Grimshaw AD. Sound-Image Data Records for Research on Social Interaction. Sociological Methods & Research. Special Issue on Sound-Image Records in social Interaction Research 1982; 11(2): 121–44.
- Pearce C, Arnold M, Phillips, C and Dwan K. Methodological considerations of digital video observation: beyond conversation analysis. International Journal of Multiple Research Approaches 2010; 4(2): 90–9. http://dx.doi.org/10.5172/mra.2010.4.2.090.
- Pringle M and Stewart-Evans C. Does awareness of being video recorded affect doctors’ consultation behaviour? The British Journal of General Practice 1990;40(340):455. PMid:2271278; PMCid:PMC1371415.
- Brewer MB. Research design and issues of validity. In Handbook of Research Methods in Social and Personality Psychology. Cambridge: Cambridge University Press, 2000:3–16.
- Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. Thousand Oaks, CA: Sage 2007.
- Montague E, Xu J, Chen P, Asan O, Barrett BP and Chewning B. Modeling eye gaze patterns in clinician–patient interaction with lag sequential analysis. human factors. The Journal of the Human Factors and Ergonomics Society 2011;53(5):502–16.
- Ong L, De Haes J, Hoos A and Lammes F. Doctor-patient communication: a review of the literature. Social Science and Medicine 1995;40(7):903–18. http://dx.doi.org/10.1016/0277-9536(94)00155-M.
- Blanchard CG, Labrecque MS, Ruckdeschel JC and Blanchard EB. Information and decision-making preferences of hospitalized adult cancer patients. Social Science and Medicine 1988;27(11): 1139–45. http://dx.doi.org/10.1016/0277-9536(88)90343-7.
- Harrison BL (Ed) Video annotation and multimedia interfaces: from theory to practice. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. Thousand Oaks, CA: Sage, 1991.
- De Lusignan S, Kumarapeli P, Debar S, Kushniruk A and Pearce C. Using an open source observational tool to measure the influence of the doctor’s consulting style and the computer system on the outcomes of the clinical consultation. Studies in Health Technology and Informatics 2009;150:1017–21. PMid:19745467.
- Cegala DJ, McGee DS and McNeilis KS. Components of patients’ and doctors’ perceptions of communication competence during a primary care medical interview. Health Communication 1996;8(1):1–27. http://dx.doi.org/10.1207/s15327027hc0801_1.
- Cromarty I. What do patients think about during their consultations? A qualitative study. The British Journal of General Practice 1996;46(410):525. PMid:8917871; PMCid:PMC1239747.
- Pearce C, Dwan K, Arnold M, Phillips C and Trumble S. Doctor, patient and computer–a framework for the new consultation. International Journal of Medical Informatics 2009;78(1):32–8. http://dx.doi.org/10.1016/j.ijmedinf.2008.07.002. PMid:18752989.
- Hermansson GL, Webster AC and McFarland K. Counselor deliberate postural lean and communication of facilitative conditions. Journal of Counseling Psychology 1988;35(2):149–53. http://dx.doi.org/10.1037/0022-0167.35.2.149.
- Roter DL. Patient participation in the patient-provider interaction: the effects of patient question asking on the quality of interaction, satisfaction and compliance. Health Education and Behavior 1977;5(4):281. http://dx.doi.org/10.1177/109019817700500402.
- Connor M, Fletcher I and Salmon P. The analysis of verbal interaction sequences in dyadic clinical communication: A review of methods. Patient Education and Counseling 2009;75(2):169–77. http://dx.doi.org/10.1016/j.pec.2008.10.006. PMid:19097842.
- Hall JA, Irish JT, Roter DL, Ehrlich CM and Miller LH. Gender in medical encounters: An analysis of physician and patient communication in a primary care setting. Health Psychology 1994;13(5):384. http://dx.doi.org/10.1037/0278-6133.13.5.384. PMid:7805632.
- Burchard KW and Rowland-Morin PA. A new method of assessing the interpersonal skills of surgeons. Academic Medicine 1990;65(4):274–6. http://dx.doi.org/10.1097/00001888-199004000-00012. PMid:2334511.
- Kraan H, Crijnen A, Zuidweg J, Van der Vleuten C and Imbos T. Evaluating Undergraduate Training –A Checklist for Medical Interviewing Skills. In: Communicating With Medical Patients. Newbury Park, CA: Sage, 1989, pp. 167–77.
- Duggan P and Parrott L. Physicians’ nonverbal rapport building and patients’ talk about the subjective component of illness. Human Communication Research 2001;27(2):299–311. http://dx.doi.org/10.1093/hcr/27.2.299. http://dx.doi.org/10.1111/j.1468-2958.2001.tb00783.x.
- Als AB. The desk-top computer as a magic box: patterns of behaviour connected with the desk-top computer; GPs’ and patients’ perceptions. Family Practice 1997;14(1):17. http://dx.doi.org/10.1093/fampra/14.1.17. PMid:9061339.
- Collins L, Schrimmer A, Diamond J and Burke J. Evaluating verbal and non-verbal communication skills, in an ethnogeriatric OSCE. Patient Education and Counseling 2011;83(2):158–62. PMid:20561763.
- D’Agostino TA and Bylund CL. The nonverbal accommodation analysis system (NAAS): initial application and evaluation. Patient Education and Counseling. 2011;85(1):33–9. PMid:20851559.
- Newman W, Button G and Cairns P. Pauses in doctor–patient conversation during computer use: The design significance of their durations and accompanying topic changes. International Journal of Human–Computer Studies 2010;68(6):398–409. http://dx.doi.org/10.1016/j.ijhcs.2009.09.001.
- Pearce C, Trumble S, Arnold M, Dwan K and Phillips C. Computers in the new consultation: Within the first minute. Family Practice 2008;25(3):202–8. http://dx.doi.org/10.1093/fampra/cmn018. PMid:18504254.
- Mast MS, Hall JA, Klöckner C and Choi E. Physician gender affects how physician nonverbal behavior is related to patient satisfaction. Medical Care 2008;46(12):1212–8. http://dx.doi.org/10.1097/MLR.0b013e31817e1877. PMid:19300310.
- Cooper JB, Barron D, Blum R, Davison JK, Feinstein D, Halasz J et al. Video teleconferencing with realistic simulation for medical education* 1. Journal of Clinical Anesthesia 2000;12(3):256–61. http://dx.doi.org/10.1016/S0952-8180(00)00148-3.
- Roter D, Frankel R, Hall J and Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Journal of General Internal Medicine 2006;21(S1):S28–34. http://dx.doi.org/10.1111/j.1525-1497.2006.00306.x. PMid:16405706; PMCid:PMC1484830.
- Carayon P. Human factors of complex sociotechnical systems. Applied Ergonomics 2006;37(4):525–35. http://dx.doi.org/10.1016/j.apergo.2006.04.011. PMid:16756937.
- Wilson JR. Fundamentals of ergonomics in theory and practice. Applied ergonomics 2000;31(6):557–67. http://dx.doi.org/10.1016/S0003-6870(00)00034-X.
- Lawler EK, Hedge A and Pavlovic-Veselinovic S. Cognitive ergonomics, socio-technical systems, and the impact of healthcare information technologies. International Journal of Industrial Ergonomics. 2011;41(4):336–44. http://dx.doi.org/10.1016/j.ergon.2011.02.006.
- Berg M. Implementing information systems in health care organizations: myths and challenges. International Journal of Medical Informatics. 2001;64(2–3):143–56. http://dx.doi.org/10.1016/S1386-5056(01)00200-3.
- Ludwick D and Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. International Journal of Medical Informatics 2009;78(1): 22–31. http://dx.doi.org/10.1016/j.ijmedinf.2008.06.005. PMid:18644745.
- Intelligent Video Solutions
- Learning Center
- Research
- Using Video Based Observation Research Methods in Health Encounters

